In a recent article entitled “A Hayekian Defense of Evidence-Based Medicine” Andrew Foy makes a thoughtful attempt to rebut my article on “The Devolution of Evidence-Based Medicine.” I am grateful for his interest in my work and for the the kind compliment that he extended in his article. Having also become familiar with his fine writing, I return it with all sincerity. I am also grateful to the THCB staff for allowing me to respond to Andrew’s article.
Andrew views EBM as a positive development away from the era of anecdotal, and often misleading medical practices: “Arguing for a return to small data and physician judgment based on personal experience is, in my opinion, the worst thing we could be promoting.” Andrew’s main concern is that my views may amount to “throwing the baby with the bath water.”
On those counts, I must plead guilty as charged. I have been trying to sink that baby for a number of years now, attacking it from a variety of angles. I have made a special plea in favor of small data and I have even questioned the intellectual sanity of EBM. On the question of the coexistence between EBM and clinical judgment, I have been decidedly intolerant, relegating EBM to second class citizen status. In other words, I’m an unapologetic EBM-denialist which, as I found out yesterday on Twitter, puts me in the same category as climate change skeptics.
My main concern today, however, is to address the relationship between EBM and the free-market, and to reject Andrew’s point that EBM is somehow compatible with it.
First, though, let me say that in no way do I deny the notion that American medicine has, for decades, harbored practices of highly doubtful benefit to patients, and that many such practices may, in fact, have been dangerous or harmful. I am fully on board with any effort to eradicate “eminence-based medicine.”
Before we reach out for an EBM solution to that problem, however, we should first wonder about causes. What keeps the errors of eminence-based medicine persisting for so long? Why do patients and doctors remain so wedded to a course of therapy as to blithely engage in un-beneficial or even harmful care?
If I read Andrew correctly, he seems to believe that these errors persist because outcome uncertainties are inherent to clinical care, hence the need for EBM.
But that cannot be the fundamental reason. Why would patients continue to pursue a treatment for which they have neither objective nor subjective tangible benefit? Why wouldn’t they refuse to go along? After all, many of them do exercise their ability to be non-compliant in the case of treatments deemed beneficial to them according to the truths of EBM!
Outcome uncertainty, then cannot be the reason why futile or harmful treatments persist, and if outcome uncertainty is not the reason, reducing it by way of EBM may not be the answer either.
What eludes Andrews is that eminence-based medicine is not simply the result of individual doctors exercising judgment with limited knowledge. Rather, eminence-based medicine happens when doctors apply their own pet theories and disregard the needs and wants of the patient at hand.
By missing that point, Andrew misses that eminence-based medicine is precisely minimized by the free-market and, on the contrary, encouraged by government intervention. The history of American medicine provides ample examples to make that point.
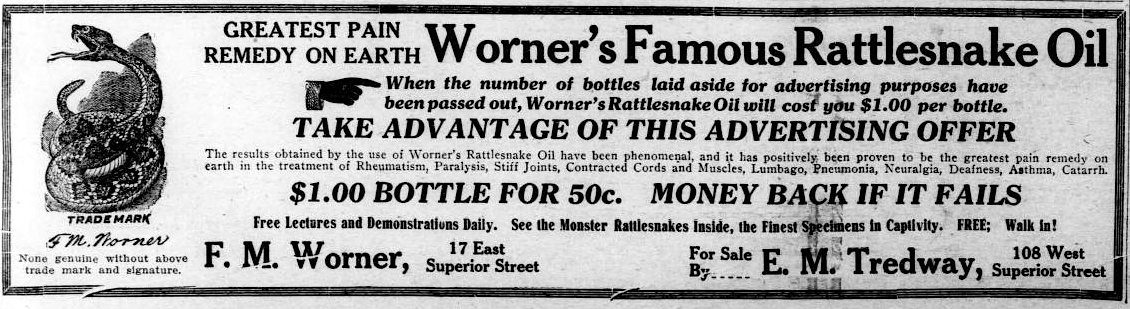
In the late nineteenth century, healthcare in the United States was uniquely unregulated. Yet, contrary to common belief or fabricated myths, care was improving by leaps and bounds, getting at once better, cheaper—and more scientific. It is during that time that some of the finest medical institutions emerged, including the Mayo Clinic and the Johns Hopkins Hospital. Sure, there were snake oil salesmen, but these were by-and-large being driven out of business by a growing community of serious, well-trained, and effective physicians. And competition among these practitioners kept them humble and at the service of patients.
All of this changed in the 1910’s when, following the Flexner reforms, state licensing laws were enacted. It is in the heels of these laws that medical paternalism emerged.
As an illustration, consider this passage excerpted from an official report published soon after the enactment of licensing laws:
The physician is the outstanding practitioner of medicine. The need and the value of his service sets him above all others. He alone, of all types of medical practitioners in the United States, is permitted by law to diagnose and treat all diseases and conditions and to use (with certain minor exceptions) any form of diagnostic or therapeutic technique which he considers necessary, desirable, and within his professional skill. (Report of the Committee on the Cost of Medical Care, 1928, p. 195)
From that point onward, medical abuses of privilege became much more widespread than they had been.
Furthermore, as Kenneth Ludmerer has pointed out, this elevation of the physician to the status of demi-God by government fiat went hand-in-hand with the rise of the academic ivory tower, since academic medical schools were producing the “cream of the crop” among doctors. Academic ivory towers, naturally, became common sources of practices founded on eminence.
Of course, licensing laws and the emergence of the ivory towers are not the only factors to consider. Other government interventions soon followed to bring about systems of third-party payment for medical care—health insurance. Without these government interventions, and without the existence of licensing laws, it is unlikely that health insurance would have emerged from the free market. By unmooring medical decisions from any financial constraints, health insurance contributes immensely to the perpetuation of eminence-based practice.
It is this regulatory context, then, that is at the root of eminence-based medicine, and not the uncertainties of clinical care which, in a profound way, are inherent to the medical encounter.
Andrew believes that EBM discovery is akin to price setting on the free market. I strongly disagree with that analogy. As Andrew himself has noted, prices set in the free market convey consumer values and are the end results of myriad decisions made on the basis of dispersed knowledge.
EBM results, on the other hand, are statistical relationships between interventions and outcomes which are carefully selected by investigators in highly contrived experimental settings. In these settings, the choices and preferences of doctors and patients are ignored or neutered by design in order to isolate the relationship of interest. Any value obtained as a result of an EBM experiment is primarily imputable to the investigators or sponsors, and only secondarily (and statistically) of benefit to patients.
EBM is no free market phenomenon. EBM is an academic invention incubated in Canada, a country with a single-payer healthcare system! As I described in my article, this invention has spun out of control and has turned EBM into a weapon wielded with equal vigor by the pharmaceutical industry, by regulators, and by those who aim to equalize the historical excesses of eminence-based medicine through the dubious doctrine of “Less-Is-More.” None of these movements, it seems, are motivated by a desire to advance a genuine human science that is meaningful to individual patients. In fact, to the extent that is a pet theory which standardizes care for entire populations, EBM is eminence-based medicine on steroids.
But if EBM is by no means a product of the free market, can the free market address our need to improve therapeutic predictions or will it set us back to a clinical stone age?
So long as narrowing clinical outcome expectations is truly desired by doctors and patients—and there is no reason to doubt that it is—then the free market is demonstrably the optimal environment that can allow human ingenuity to devise clever ways and methods to achieve that goal. But what shape or form would those methods take and how closely would they resemble what we now take to be evidence-based science, I have no idea. If I believed I held that knowledge, I would be repudiating Hayek.
Nice article. You bring up some interesting points, as usual.
After reading this article, and that of Dr Foy’s (from a fairly neutral stand point – I think) I have to say that I’m swayed more by the latter.
2 points that I think are crucial:
1) You mention that outcome uncertainty cannot be reason why futile/harmful treatments exist – but the reason you have given is in form of question – why would pt stay with Tx that had no tangible benefits (Implying that there IS indeed a benefit – correct me if I misinterpreted you)? It seems to me that this is not a complete logical argument (although I’ve not slept well last night so may be my own dull sleep deprived intellect). In fact it’s probably precisely b/c of unclear benefit that pts remain on futile Tx…Dr said this should help and so they take it (out of desperation of curing -blank- illness). This blind faith causes all kinds of harm not only in health care (eg. Trump for Pres) – Driven by the fact that neither physician nor patient (assuming eminence/expert-opinion based approach) knows whether there is benefit or harm being done.
2) when you mention def’n (or connotation) of eminence based medicine includes “disregard the needs and wants of the patient at hand.” , it seems that this is also a bit of an assumption. Eminence based medicine does not necessarily imply that the expert disregards the needs and wants of the patient. After all how do you know what that particular practitioner is thinking? Rather, eminence based medicine is no more or less than expert medical opinion, full stop. This is important b/c the proposed cure as per Dr Foy is to inform that opinion with evidence (which is a logical solution – albeit not the only solution). Whereas in your scenario, you propose free-market as the cure (which indeed would be reasonable IF the assumption in your scenario was true – which is not always the case).
Anyhow, I’m wondering if this sort of discussion (for vs against ebm) is a bit too narrow. Folks seem to assume that pro-ebm-ers ignore the patient in front of them, but at the same time poo poo small data folks as if they ignore science. Can’t a clinician use evidence (science) to inform their practice in a patient-oriented manner? Some take the approach of changing the name ebm to science-based-medicine, perhaps that might help stop the back and forth?
https://www.sciencebasedmedicine.org/about-science-based-medicine/
My (non-expert) thought is – let that which is opinable be in harmony with the intelligible, not at odds with it. Indeed Plato might say it’s like comparing apples with oranges…they are completely separate beasts.
Jacob
Hi Jacob,
Thank you for your comments and interest.
Briefly, on your point 1), and following Murray Rothbard’s classic paper (https://mises.org/library/toward-reconstruction-utility-and-welfare-economics-0) I would say that yes, in an environment where patients are given full freedom of choice, if they choose to continue a given treatment, then they demonstrate by their action that they derive some benefit from it, or that they value the treatment more than other alternatives known and available to them. And that’s true regardless of whether that benefit can be objectively identified. For you (or anyone) to say that they do not derive benefit assumes that you can get into their minds and fully comprehend their subjectivity, which is impossible and, in fact, unscientific.
The problem with eminence-based medicine then is that the patients’ freedom of choice has been greatly restricted and they are being confused “from the top” as it were, as to what is in their best interest, as opposed to being allowed to express their own interest by their free actions. Of course, many people will argue that the academic-government complex should interfere in people’s action because it knows best what is in people’s best interest. That of course, is a major assumption that is frequently shown to be wrong after the fact.
On point 2), the only way to find out the best way to inform patients is to do it in a setting with competing methods of evidence, and let people decide. That is what I conclude at the end.
On the point of making the debate too simplistic (us versus them), I may elaborate on this in a future post 🙂
Michel
Your point is well taken on point number 1 – that I cannot (nor anyone other than the patient) determine whether a given person derives benefit from a given tx. However to play devil’s advocate, knowing myself, I can say that I take a multivitamin daily. Your theory would conclude that I therefore benefit from it (based on my chosen action to take it)? However I neither subjectively appreciate any benefit from it, nor is there any measureable or objective evidence that it benefits me … yet I continue to take it. I think this is where the assumption you make differs slightly from Rothbard’s. As per his paper (in the link you provided) – the theory states “actual choice reveals, or demonstrates, a man’s preferences”. I totally agree with this. The issue is that despite it being my preference (or value) to take a daily multivit, I may not actually be benefitting from taking it (at least not subjectively or objectively…that we know of). If I dig deep, I suppose I explain my choice to take it is due to the hope/belief that it MAY confer benefit (whether or not it actually does is an unknown). But perhaps I’m knitpicking on this point.
I am with you on your second point you make. I am actually in support of competing methods of evidence. As I said, I think the debate is too narrow. Many more ways of knowing than simply what EBM would have us believe. Looking forward to your future post on this!
Cheers
Jacob
Yes, Jacob, your taking the vitamin demonstrates that you value taking more than the alternatives, even if you cannot articulate what that value or benefit is to you. Cheers, Michel
Évidence fluctuates with innovationt and progress. Setting evidence based medicine as a standard for medical care equates to building a hospital on a swamp… or to adding another deadly tool for bureaucratic rationing of novative therapy.
Excellent way of putting it!