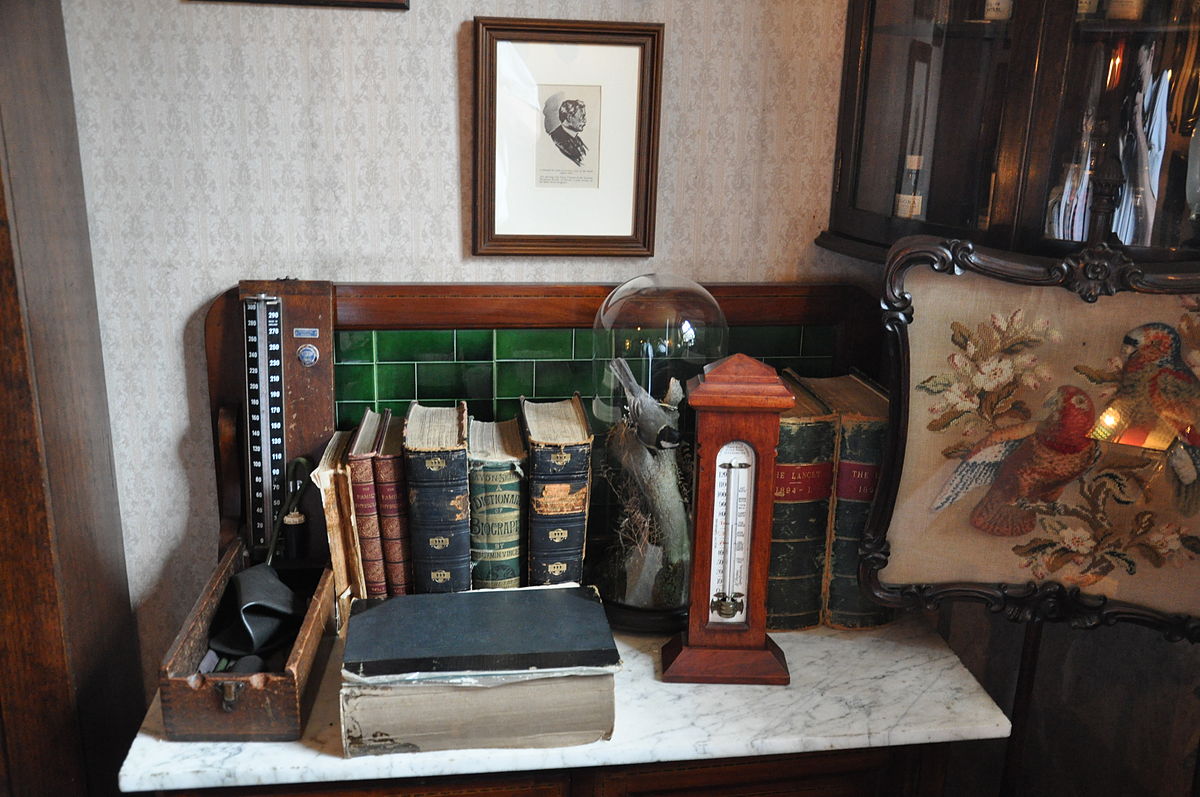
To summarize W’s case up to March 17, here were the salient features:
- Baseline signs of conduction system disease
- Progressive, and now severe, dyspnea on exertion
- Unexplained relative hypotension, not due to adrenal insufficiency
- Weight loss and early satiety
- Hypercalcemia, initially mild, now more pronounced, with suppression of PTH
- Markedly active urinary sediment with severe dipstick proteinuria, but also microscopic hematuria and calcium oxalate stones
- Worsening renal function, possibly pre-renal azotemia.
The 50-mile distance separating W from my office made frequent visits impractical, but from March 17 onward I was essentially on daily contact with the patient either by phone or email.
I could not tie everything together, but the thought occurred to me that he might have systemic sarcoidosis with cardiac involvement: hypercalcemia, heart block, shortness of breath, gastrointestinal symptoms. In fact, I was clearly hoping for this diagnosis as something potentially treatable in what otherwise looked like an ominous illness.
On March 19, however, a 2-view chest x-ray was normal and the light bulb that had gone off in my head a few days before was quickly burnt.Continue reading “From DPC to CPC – part 2”