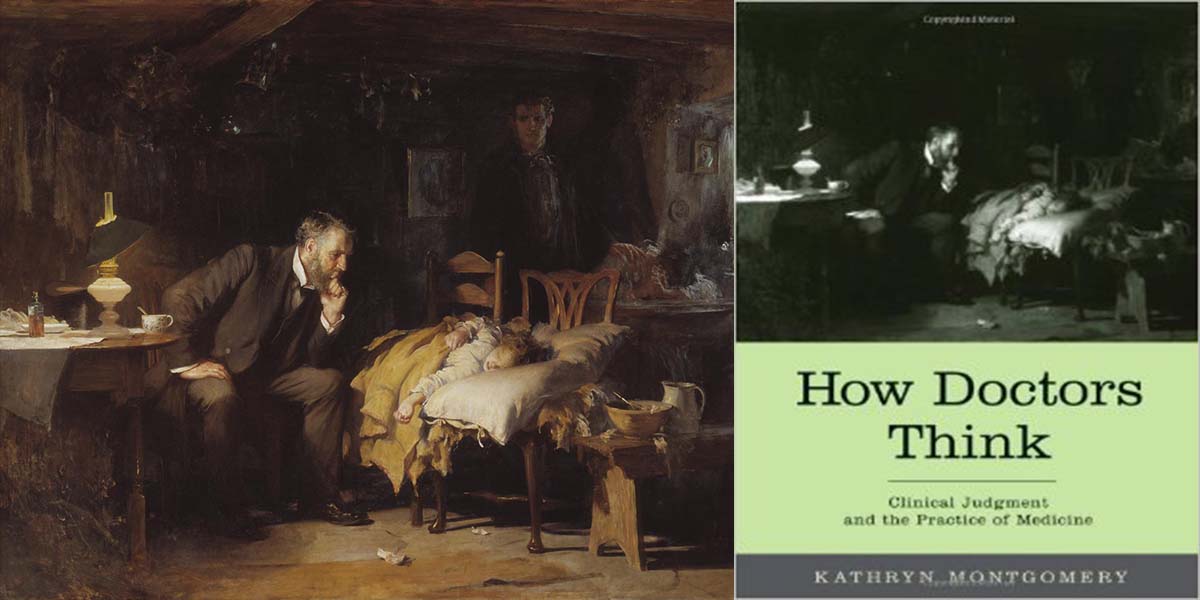
Kathryn Montgomery’s How Doctors Think: Clinical Judgment and the Practice of Medicine is an excellent book that was brought to my attention by Dr. James Gaulte in the comment section of my post on phronesis. Indeed, much of Montgomery’s monograph deals with the Aristotelian concept of practical wisdom applied to clinical decision-making.
The author is Professor of Medical Humanities and Bioethics and Professor of Medicine at Northwestern University Feinberg School of Medicine. Her book is too rich to cover deeply in a short review, but I’d like to highlight some of its major strengths as well as a few minor weaknesses.
In the first part of the book, Montgomery thoroughly demolishes the notion that medicine is applied science. Medical practice does not deal with the “unambiguous regularities of Newtonian science.” Yet, medicine-as-applied-science is a common misconception held by the medical community. According to Montgomery, to consider medicine in this way is a “misdescription.” Medicine is neither art nor science, but “science-using practice.” A failure to recognize this is a failure to understand what we do.
Part II of the book has excellent passages discussing the tenuous concept of “cause” in medicine. Sometimes we can point to a particular etiological factor and to a causal link of events leading from the etiology to the symptoms. Many times, we identify as cause what is really shorthand for a recognized pattern, i.e., a diagnostic label.
Montgomery ties her treatment of the medical concept of cause to the indispensable need for narrative in medical care. Patients and doctors alike need to forge a story of the disease, and that story must rest on some perceived causal chain of events. (As an aside, Montgomery seems to misunderstand the Aristotelian notions of material and formal causality, which she explains in a footnote, but this is a minor point and does not impact the chapter or the book in any major way).
This part of the book also contains a very good chapter on the limits of so-called evidence-based medicine, where the author highlights the problem of “particularizing” the results of clinical trials to individual patients.
Part III of the book deals with the formation of clinical judgment. Montgomery examines the various tricks of the trade that seasoned clinicians have described over the decades to illustrate the process of medical reasoning. She elaborates on Sutton’s law, the law of parsimony, the aphorism of hoofs and zebras, and the like.
The discussion is excellent, but here we must confront an inherent difficulty: much of the material is derived from experience obtained over decades during which medicine has, in fact, “misdescribed” itself as applied science. The formation of clinical reasoning, therefore, could potentially be colored by that misrepresentation. For example, reasoning priorities might not be the same if clinical judgment were formally considered as “science-using practice” and evaluated according to the virtue of phronesis.
Montgomery actually understands that point and devotes a passage to “phronesiology.” The exploration of that concept, however, is limited. In that regard, the author may not be familiar with the field of naturalistic decision making developed by Gary Klein and to which I refer to in my post on how experts decide. I think Klein’s work greatly enhances our understanding of how good decisions are made, “phronetically-speaking,” and it would have been helpful to see it mentioned here. (Also absent is a reference to Mutton’s Law, discovered by Herb Fred, which admirably captures the essence of phronetic decision-making.)
Part IV examines the nature of medicine and of the patient-doctor relationship. It is more philosophical and provides much food for thought. In one of the last chapters, Montgomery seems to reject the metaphor of the “physician as friend” which I borrowed from Edmund Pellegrino and from others who have advanced it (these philosophers are quoted at length in this part of the book). Montgomery believes that friendship is not what patients want since they typically look for medical figures of authority, and authority is not a feature of friendship.
Instead, she favors a metaphor of the “physician as neighbor” which she believes better captures the essence of the relationship. Our disagreement may be a matter of semantics because medical friendship need not imply conviviality and, if understood in a general sense (“a relationship of two people coming together for the sake of a transcendent third”), could accommodate a figure of authority. Plus, we could likewise raise a similar objection to her doctor-as-neighbor model, since that model also needs to be qualified to fit into the reality of medical care. At any rate, this is a rather minor point (and, for me, a concept in evolution).
One self-serving criticism of Montgomery’s book is that it fails to mention why the misdescription of medicine-as-science persists so tenaciously. After all, if the idea is so wrong, why is it still confusing us? As I described in my previous post on Flexner versus Osler, the regulatory history of medicine is important to understand how positivism became permanently embedded into medical education.
How Doctors Think is an outstanding reference, indispensable to anyone interested in obtaining a deeper understanding of the essence of medical care. Another review was published in JAMA when the book was released and can be found here.
[Related post: Is medicine a scientific enterprise?]