If concepts could get awards, then “risk factor” would surely be a Nobel prize winner. Barely over 50 years of age, it enjoys such an important place in medicine that I suspect most of us doctors could hardly imagine practicing without it. Yet, clearly, the concept is not native to our profession nor is its success entirely justified.
A few years ago, on the occasion of the risk factor’s fiftieth anniversary, my colleague Herb Fred and I published an editorial highlighting some of the problem with the use of this concept. I will summarize here some of those points.
The risk factor concept was developed in the first decades of the twentieth century from within the life insurance industry as it began to systematically apply statistical methods in order to optimize actuarial predictions. The idea was to identify which baseline characteristics held by individuals would correlate with future risk of death.
The Framingham investigators imported this idea into the public health sphere and introduced the term risk factor in the medical literature in 1961. From then on, the concept and term have enjoyed an unmitigated success.
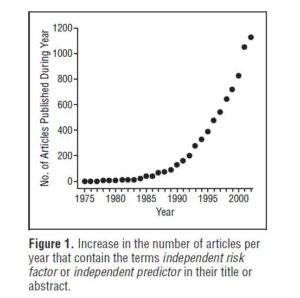
Originally confined to the cardiovascular arena, the concept is now thriving in every single medical discipline. The diagram below is from a 2005 paper by Brotman et al. The authors found that close to 1,200 papers per year claim new knowledge about “independent” risk factors. In the field of cardiovascular medicine alone, 105 such risk factors have been identified.
Furthermore:
–Risk factors, which can only make statistical claims, have morphed into full-fledged diseases. For example, hypercholesterolemia is not a naturally identifiable entity but a construct established by fiat on the basis of arbitrarily chosen cut-off numbers. Yet its disease status is widely embraced and it is sanctioned by an ICD code.
–The “diseasification” of risk factors has potential to cause harm by virtue of the so-called labeling effect. For example, it is well established that the incidence of headaches can be increased simply by affixing a label of hypertension to a person. Work absenteeism is also higher after patients are told they have high cholesterol levels.
–Risk factors garner plenty of attention even if their potential contribution to clinical outcomes is minuscule. One example is hypertriglyceridemia, whose independent contribution to the risk of cardiac disease is still debated. Obesity also barely increases cardiovascular risk when considered in isolation, and it may even be preventive in certain situations. Such attention to trivial risk factors may benefit the public health sector and the pharmaceutical industry, but whether patients are actually served remains to be seen.
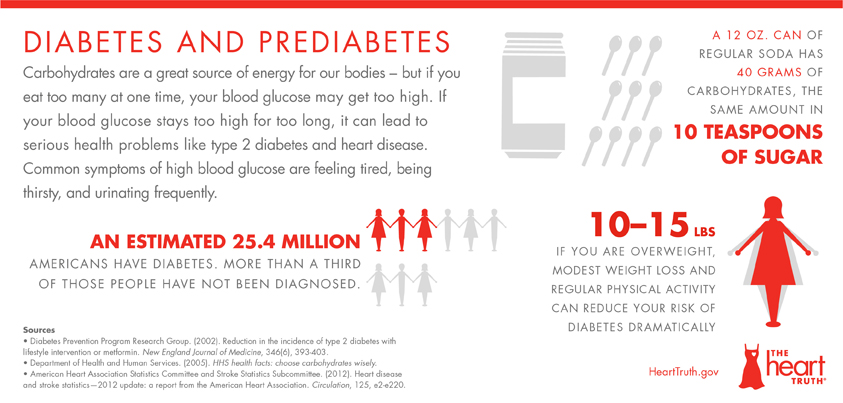
–The incidence of risk factors is further increased by the establishment of “pre” conditions such as pre-hypertension and pre-diabetes. New risk factors can also be concocted by combining other risk factors, e.g., the so-called metabolic syndrome. Many newcomers are “proto risk factors,” i.e., risk factors for risk factors. One example is “normal weight obesity,” which is a risk factor for the metabolic syndrome.
–Frequently, the relationship between risk factor and clinical outcome is not as straightforward as claimed. For example, fatality rates for stroke have been in steady decline since the beginning of the twentieth century, long before any mechanism was available to identify or reverse its related risk factors. Likewise, careful analysis of life insurance data shows that coronary mortality has been declining since the mid 1950’s, before risk factor prevalence started to fall. Some risk factors, like hypertension, may have a “U-shaped” relationship to outcomes.
–Finally, as we now know from randomized clinical trials, risk factor modification is itself risky, as demonstrated by the trials of clofibrate, hormone replacement therapy, torcetrapib, rosiglitazone, to name but a few examples.
Risk factors have become the principal justification for turning medical care into a public health activity. Using risk factor modification as a surrogate for quality of care, doctors are given incentives to treat patients according to statistical norms. As we have shown in the paper, there is sufficient ambiguity to warrant caution against the widespread use of such a powerful concept.
[Related post: Risk factors, causes, and the diet-lipid hypothesis]
[Related post: Population medicine: the other ‘dismal science’]
P.S. Anyone interested in obtaining the list of 53 references used in the editorial should feel free to contact me.
Every once in a while, I speak up to politely challenge someone’s claim of how a risk factor caused a death or disease state, though they obviously don’t use the vocabulary ‘risk factor,’ but speak of it as part of the disease process. I usually find out risk factors have gained a sacred status to many people.
Indeed. I’m actually amazed at how much the phrase itself has metastasized in business and popular culture.
The article points in this direction but I don’t think fully explores the confusion of risk factors with causes. A risk factor is something that is associated with an actual illness (and for that to make sense we need to excluded what the author calls diseasified risk factors from the category of illness). Association can come about in many ways. Some risk factors like smoking truly do cause disease. But the association can also come about because the disease caused the marker to be elevated, or some other factor (maybe not known at this time) caused both the disease and the marker. Finally the association may come about through confounding variables, or just by accident. A lot of the harm of this thinking comes about from treating the entire category of associations as if they were causes. The author mentions risk factor modification — there is no good reason to expect, for example that trying to influence a blood marker that was an effect, or linked through a confounder, would have any benefit.
You’re correct, Robert. The topic of causality requires its own treatment and cannot be dealt with quickly. That said, it’s well recognized in medical circles that association are not necessarily causative. Establishing causation, however, is another story.
“Obesity also barely increases cardiovascular risk when considered in isolation, and it may even be preventive in certain situations.”
I’m curious how obesity can be protective against heart disease. I know of one person who just turned 90 and is obese. He seems to be the exception in that age bracket.
Google “obesity paradox” and a number of scholarly articles should pop up. There is no causal mechanism identified or agreed upon. It’s not the kind of phenomenon that ever gets a definitive explanation.