If anyone has any lingering doubts that the promises of evidence-based medicine are quickly evaporating, the recent blog post by Larry Husten on the statin war should quickly dispel them. Husten gives an excellent account of the latest battle opposing the pro- and the anti- camps.
What happened?
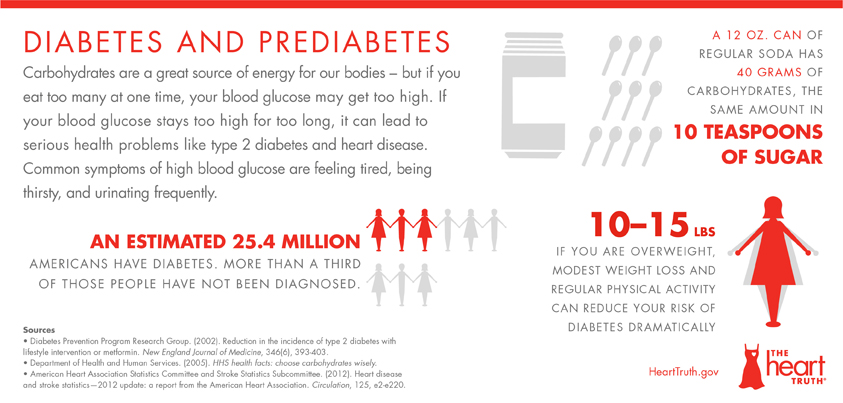
The pro-statinists published a 30-page diatribe in The Lancet. Statins save lives, they assert. The evidence is incontrovertible. Yes, they can have side effects such as muscle pain, no one disputes that. But drawing attention to those side-effects—as the anti-statinists do—endangers patients who now find a reason to refuse to take the life-saving drugs. There’s evidence of that happening.
The anti-statinists voiced their position in the BMJ. Statins cause muscle pain and fatigue, they assert. The evidence is incontrovertible. Yes, they can save lives, no one disputes that. But trumpeting the benefits or down-playing the harm—as the statinists do—prevents patients from partaking in the glorious activity of “shared-decision making.” There’s evidence of that happening.Continue reading “Three cheers for the statin war”